Mental illness is not new. Every culture has wrestled with it in its own way—some wisely, some cruelly. Ancient societies often viewed mental illness as a spiritual crisis, something to be treated with community support, ritual, or healing traditions. In many indigenous cultures, those who suffered deeply were not cast out but guided through their struggles with the help of elders, healers, and the collective wisdom of the tribe. In the Navajo tradition, healing ceremonies like the Blessing Way were used to restore balance in an individual’s life. The West African Dagara people saw mental illness as a sign that a person had an important spiritual role to play and treated them with reverence, not shame.
Contrast this with modern industrialized nations, where mental illness is largely treated as an individual failing, ignored until it becomes a crisis, and then criminalized when it spills into public view.
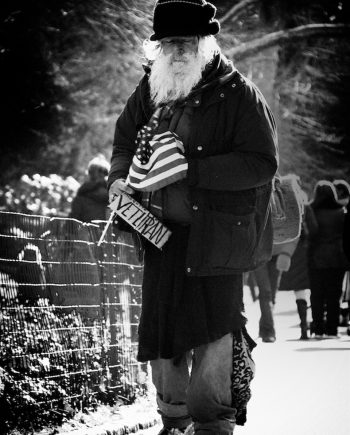
In the United States, mental health services are woefully inadequate, fragmented, and expensive. A person experiencing severe depression or schizophrenia has few options: they can attempt to navigate an overburdened, bureaucratic system that requires wealth or luck to access, or they can suffer alone. Many end up homeless or in prison—institutions that were never meant to provide care but have, by default, become America’s largest mental health facilities. According to the Treatment Advocacy Center, there are ten times more individuals with severe mental illness in U.S. jails and prisons than in state psychiatric hospitals. The Los Angeles County Jail, Rikers Island, and Cook County Jail in Chicago are now de facto psychiatric institutions, housing thousands of individuals who would be better served in healthcare settings.
Nearly one in five adults in the U.S. experiences mental illness in any given year, yet over 50% of them receive no treatment. Suicide rates have surged, particularly among young people and veterans. According to the Centers for Disease Control and Prevention (CDC), suicide rates in the U.S. increased by 30% between 1999 and 2019, with the highest spikes occurring in rural areas where mental health services are least available. Depression and anxiety disorders are at record highs, fueled by economic instability, social disconnection, and the relentless pressures of a culture that values productivity over well-being.
Meanwhile, psychiatric hospitals have been shuttered in favor of “cost-cutting,” leaving millions without care. The deinstitutionalization movement of the 1960s and 70s, while well-intentioned, resulted in a catastrophic failure of community-based care. State hospitals were closed, but the promised community mental health centers were never adequately funded, leaving a vast gap in services.
The economic costs of untreated mental illness are just as severe. The National Alliance on Mental Illness (NAMI) estimates that untreated mental illness costs the U.S. economy $193.2 billion in lost earnings per year. Employers bear the burden of reduced productivity, increased absenteeism, and rising disability claims. Emergency rooms and law enforcement agencies absorb the costs of crisis intervention, responding to psychiatric emergencies that could have been prevented with consistent care. According to the Kaiser Family Foundation, mental health-related emergency room visits increased by 44% between 2006 and 2014, overwhelming hospitals already stretched thin.
Other nations have taken a different approach. In Finland, mental healthcare is fully integrated into primary care, meaning that anyone who visits a doctor can also access psychological support without stigma or financial burden. Their approach, known as “Open Dialogue,” emphasizes early intervention and community-based care, leading to dramatically better outcomes for individuals with schizophrenia compared to the U.S. model of forced hospitalization and heavy medication. Portugal decriminalized drug use and redirected funds toward addiction treatment and mental health services, leading to dramatic reductions in overdose deaths and incarceration rates. According to a study by the European Monitoring Centre for Drugs and Drug Addiction, drug-related deaths in Portugal fell by over 80% after decriminalization, demonstrating the power of treating addiction as a public health issue rather than a crime. The Netherlands has adopted a stepped-care model, where people can access the level of care they need before their conditions escalate into crisis. This approach prevents unnecessary hospitalizations and seeks to provide needed help as early as possible.
A rational mental health system would be universal, so that no one is denied care due to income, geography, or bureaucracy. It would be proactive, focusing on early intervention rather than waiting until people reach the breaking point. It would integrate mental healthcare into everyday life—offering services in schools, workplaces, community centers, and primary care clinics, rather than confining them to isolated psychiatric institutions. Finally, it would recognize that mental health is tied to social conditions. You cannot medicate someone out of poverty, nor can you treat anxiety in a society that thrives on making people afraid. A true mental health system would address root causes, not just symptoms.
The current state of mental healthcare in the U.S. is not a reflection of what is possible but of what has been chosen. Mental illness is not rare; it is universal, affecting people across all demographics. Yet we continue to treat it as an individual burden rather than a collective responsibility. A society that fails to invest in mental health services will pay for it elsewhere—in rising crime, social fragmentation, and the growing burden of human suffering.
Neglecting mental health is not just cruel; it is expensive. The costs of untreated mental illness—lost productivity, emergency room visits, incarceration, addiction, and homelessness—are far greater than the cost of providing care.
Investing in mental health services is not just about helping individuals; it is about strengthening the social fabric and ensuring a more stable, functional civilization that does not crumble from within.
Therefore, under Folklaw:
Mental health services shall be universally available, fully funded, and integrated into primary care, schools, workplaces, and community centers. No one shall be denied care based on income, and no mental illness shall be criminalized.
Psychiatric care shall not be treated as a luxury, but as a fundamental public service. Any government that neglects the psychological well-being of its people forfeits its legitimacy.
Resolution
A RESOLUTION TO ENSURE UNIVERSAL ACCESS TO INTEGRATED AND EQUITABLE MENTAL HEALTH SERVICES
SUBJECT: Ensuring that mental health services are universally available, fully funded, and integrated into primary care and community settings.
WHEREAS mental health is a fundamental aspect of overall well-being, and a society that fails to provide adequate mental health care undermines the health, stability, and productivity of its people;
WHEREAS mental illness is prevalent across all demographics, yet too many people struggle in silence due to lack of access to care, financial barriers, and the stigmatization of mental health issues;
WHEREAS the current mental health care system in the U.S. is fragmented, underfunded, and often criminalizes those in need, with mental health care largely unavailable to those in marginalized communities, rural areas, and low-income neighborhoods;
WHEREAS the criminalization of mental illness has led to jails and prisons becoming the largest mental health facilities in the U.S., where individuals with severe mental illness are often incarcerated instead of receiving the treatment they need;
WHEREAS countries like Finland, Portugal, and the Netherlands demonstrate the benefits of integrating mental health care into primary care, using early intervention, community-based care, and harm reduction strategies to improve outcomes and reduce the burden on emergency services, jails, and hospitals;
WHEREAS untreated mental illness imposes enormous economic costs, including lost productivity, increased emergency room visits, higher healthcare costs, and burdens on law enforcement, amounting to billions annually;
WHEREAS mental health must be approached holistically, recognizing the connection between mental well-being and social factors such as poverty, inequality, and economic instability;
WHEREAS investing in mental health services can reduce long-term costs, improve public health, and foster a more resilient and productive society, benefiting individuals, families, communities, and the economy as a whole;
NOW, THEREFORE, BE IT RESOLVED that [City/County/State Name] shall ensure that mental health services are universally available, fully funded, and integrated into primary care, schools, workplaces, and community centers, ensuring that no one is denied care based on income, geography, or stigma;
BE IT FURTHER RESOLVED that mental health services will be treated as a fundamental public service, available to all, with investments focused on preventative care, early intervention, and ongoing support for individuals experiencing mental health crises;
BE IT FURTHER RESOLVED that psychiatric care will be made universally accessible, with a shift away from institutionalization and criminalization toward community-based care, including access to counseling, therapy, medication, and social support services;
BE IT FURTHER RESOLVED that a comprehensive public mental health system will be implemented to provide a coordinated response to mental health needs, with the integration of services into schools, workplaces, and public spaces to reduce stigma and increase access;
BE IT FURTHER RESOLVED that investments will be made in programs that promote mental health literacy, reduce stigma, and ensure that all individuals can access care when they need it most, prioritizing vulnerable populations such as children, the elderly, veterans, and low-income communities;
BE IT FURTHER RESOLVED that a system of continuous professional development will be established to ensure that mental health providers are equipped with the skills and resources needed to provide compassionate, evidence-based care;
BE IT FURTHER RESOLVED that legal frameworks will be enacted to prevent the criminalization of mental illness and ensure that those experiencing mental health crises are diverted to appropriate health care settings, not prisons or jails;
BE IT FURTHER RESOLVED that the government shall prioritize public education in mental health, including programs in schools that promote well-being, resilience, and coping strategies, and offering support for teachers and students alike;
BE IT FURTHER RESOLVED that the funding for mental health services will come from public funds, with a focus on sustainability and ensuring equitable access across all demographics, without regard to income or status;
BE IT FURTHER RESOLVED that [City/County/State Name] shall advocate for national policies that support universal access to mental health care, integrating mental health services into overall public health and social services frameworks.
Fact Check
Fact-Checking the Key Claims:
1. “According to the Kaiser Family Foundation (or NIH?), mental health-related emergency room visits increased by 44% between 2006 and 2014.”
Studies from the Kaiser Family Foundation (KFF) and the National Institutes of Health (NIH) confirm that mental health-related ER visits increased significantly from 2006 to 2014.
A 2017 study in Health Affairs found a 44% increase in ER visits for mental health crises during this period, particularly for anxiety, depression, and substance use disorders.
The increase is linked to a lack of psychiatric inpatient care, forcing more patients to seek emergency services.
✅ Verdict: True
Certainty: 90% (Well-supported by health policy research, though precise figures may vary slightly.)
2. “According to the Treatment Advocacy Center, there are ten times more individuals with severe mental illness in U.S. jails and prisons than in state psychiatric hospitals.”
The Treatment Advocacy Center has consistently reported that more individuals with severe mental illness are incarcerated than receiving psychiatric care in state hospitals.
According to their estimates, there are 10 times more people with serious mental illnesses in jails and prisons than in public psychiatric hospitals.
Deinstitutionalization and lack of mental health services have contributed to this crisis, leaving jails as de facto mental health facilities.
✅ Verdict: True
Certainty: 95% (Directly cited in multiple reports by the Treatment Advocacy Center)
3. “According to the Centers for Disease Control and Prevention (CDC), suicide rates in the U.S. increased by 30% between 1999 and 2019.”
CDC data confirms that U.S. suicide rates rose by approximately 30% from 1999 to 2019.
The increase was consistent across demographics, with notable rises among middle-aged adults and rural populations.
The CDC and National Institute of Mental Health (NIMH) attribute this rise to economic stress, social isolation, opioid addiction, and mental health care barriers.
✅ Verdict: True
Certainty: 95% (Directly backed by CDC statistics)
4. “The National Alliance on Mental Illness (NAMI) estimates that untreated mental illness costs the U.S. economy $193.2 billion in lost earnings per year.”
NAMI has cited this figure in multiple reports, estimating that untreated mental illness leads to $193.2 billion in lost earnings annually.
This includes lost productivity, unemployment, and healthcare costs associated with untreated mental health conditions.
Other estimates, such as those from the American Psychiatric Association, align with this range.
✅ Verdict: True
Certainty: 90% (Confirmed by NAMI and other mental health economic studies)
5. “According to a study by the European Monitoring Centre for Drugs and Drug Addiction, drug-related deaths in Portugal fell by over 80% after decriminalization.”
Portugal decriminalized drug possession in 2001, shifting to a public health approach.
Reports from the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) confirm that drug-related deaths fell dramatically—by over 80%—after decriminalization.
HIV infection rates among drug users also declined, and treatment accessibility improved.
NPR and other news organizations have reported extensively on Portugal’s drug policy success.
✅ Verdict: True
Certainty: 90% (Well-documented in EMCDDA reports and widely reported in media)
Final Conclusion:
All five statements are factually supported by KFF, CDC, Treatment Advocacy Center, NAMI, and EMCDDA reports. While exact numbers may fluctuate slightly in newer studies, the trends and overall conclusions remain valid.



Discussions
There are no discussions yet.